Case:
29-year-old female presents with two days of worsening abdominal pain described as “bloated”, “tight”, and “sharp”. She reports associated shortness of breath, nausea, vomiting, and inability to tolerate P.O. Recently underwent egg retrieval during infertility treatment.
Physical Examination:
Afebrile, BP 109/72, HR 93, O2 98%, RR 18
Uncomfortable, diffusely tender, but soft abdomen. Mildly distended. No rebound or guarding.
Labs:
B-HCG negative
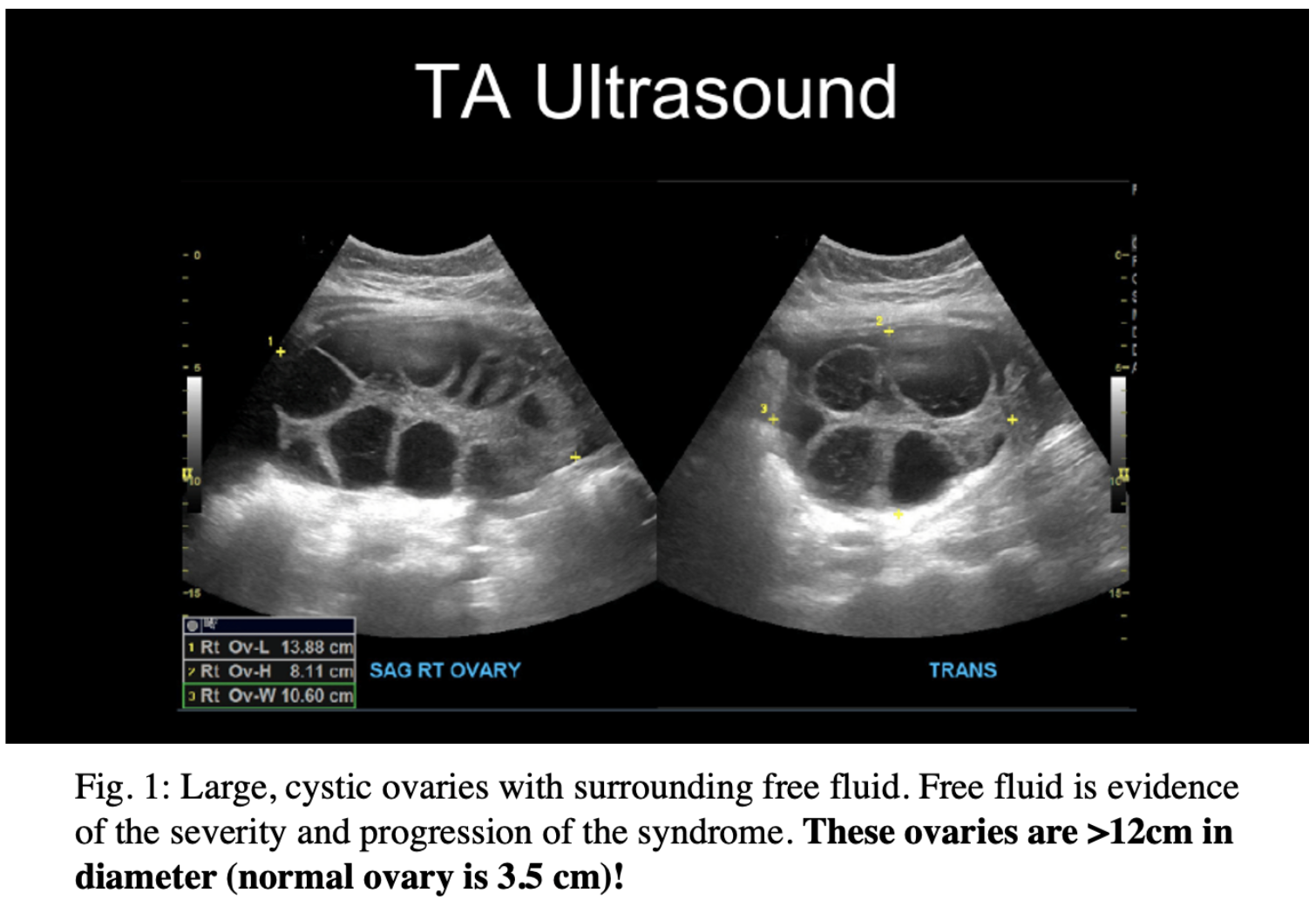
You decide to perform a bedside transabdominal (TA) pelvic ultrasound…
Diagnosis
You suspect possible ovarian hyperstimulation syndrome (OHSS). The most important data comes from imaging – particularly ultrasound! Key findings include pathognomonic cystic ovaries with associated free fluid. In severe cases, ascites, hydrothorax, or even hydropericardium can be found. Beyond imaging, labs can be significant for a reactive leukocytosis, transaminitis, and electrolyte imbalances secondary to the third-spacing and associated hypovolemia. Acute renal injury in the setting of hypovolemia can also be seen in severe cases.
OHSS POCUS Findings
Let’s dive into some POCUS findings. Clinically, there are varying degrees of OHSS. The severe form has pretty profound clinical and sonographic findings. Severe abdominal pain is accompanied by a large amount of free fluid on abdominopelvic assessment. The ovaries are enlarged >12cm in diameter and contain numerous large thin-walled cysts which obliterate the normal ovarian parenchyma. Evaluation of the blood flow to the ovaries is crucial in these patients due to their increased risk for ovarian torsion.
Rapid Review
Hyperstimulated ovaries are a normal response to elevated circulating HCG levels. Ovarian hyperstimulation syndrome (OHSS) is a term used when there is associated fluid shifts. This complication can be found in as many as 5% of patients receiving assisted reproductive technology. In those undergoing reproductive-assistive therapy, ovulation is induced through injections of human chorionic gonadotropin (hCG) or oral medication such as clomiphene or letrozole. These agents increase the maturation of multiple follicles, allowing for more eggs to be released in a single cycle. However, this rapid augmentation of ovulation leads to a significant inflammatory response. This response can result in both follicle rupture and increased vascular permeability, creating the third-spacing responsible for the symptoms of OHHS. These symptoms range from abdominal pain and distention to frank ascites with associated organ failure.
Management
While the disease progression can be rapid, it is self-limited. Management should be centered on monitoring for progression of symptoms and supportive care, i.e. appropriate hydration and pain management. During this time patients are encouraged to limit physical activity to reduce risk of rupture and ovarian torsion. In the rare event patients progress to severe organ dysfunction, hospitalization will be required and the goal transitions to prevention of decline. This will require careful maintenance of hemodynamics, avoiding extremes such as hemoconcentration.
Case Conclusion
The patient was admitted for abdominal pain. She underwent imaging that revealed significantly enlarged ovaries bilaterally, as well as ascites, and was diagnosed with ovarian hyperstimulation syndrome. There was low suspicion of ovarian torsion. The patient was noted to have mild hyponatremia which was corrected by HD#2. She received pain medication and anti-emetics. Her electrolytes were monitored and corrected as needed. She underwent two US evaluations assessing for possible paracentesis, but no significant fluid pockets could be found. The patient's pain management regimen was optimized, and by HD#4, her pain was well controlled on PO agents. Given normal vitals, normal electrolytes, and improved pain, patient was deemed stable for discharge to home to follow up at clinic in one week with OBGYN.
References:
1. Kumar, P., Sait, S. F., Sharma, A., & Kumar, M. (2011). Ovarian hyperstimulation syndrome. Journal of human reproductive sciences, 4(2), 70–75. https://doi.org/ 10.4103/0974-1208.86080
2. American Society for Reproductive Medicine. Prevention and treatment of moderate and severe ovarian hyperstimulation syndrome: a guideline Practice Committee of the American Society for Reproductive Medicine. https://www.asrm.org/globalassets/asrm/asrm-content/ news-and publications/practice-guidelines/for-nonmembers/prevention_ and _treatment_of_moderate _to_severe_ohss.pdf
3. Busso C, Soares S, Pellicer A. Pathogenesis, Clinical Manifestations and Diagnosis of Ovarian Hyperstimulation Syndrome. April 2019. https://www.uptodate.com/contents/ pathogenesis- clinical-manifestations-and-diagnosis-of-ovarian-hyperstimulation-syndrome. Accessed September 17, 2020.
4. Chin-Der Chen, Ming-Ying Wu, Kuang-Han Chao, Yih-Ron Lien, Shee-Uan Chen, Yu-Shih Yang. (2011). Update on management of ovarian hyperstimulation syndrome. Taiwanese Journal of Obstetrics and Gynecology, Volume 50, Issue 1, 2011, Pages 2-10, ISSN 1028-4559, https://doi.org/10.1016/j.tjog.2011.01.014.
5. Rumack, Carol L Deborah. Abdominal and Pelvic Sonography. In: Diagnostic Ultrasound. Vol 1. 5th ed. Elsevier; 2018:572.
About the Authors:
Allyson Hansen is the Ultrasound Director for USF EM residency
Charlotte Derr is the Program and Ultrasound Director for USF EM residency
Caitlyn Johnson is a medical student in the 2023 class of the Morsani College of Medicine
(727)363-4500
|
CREATE ACCOUNT
|
LOG IN
|
CART
|
Item(s) added to cart
Proceed to Checkout
Continue Shopping