Ultrasound Guided Nerve Blocks
Introduction / Summary
Common discussion throughout the United States healthcare community in the past few years has been regarding the “opioid epidemic” and how its plaguing both soldiers and civilians with addiction, withdrawal, depression of cognitive abilities, and other common side effects. In the fight for freedom, it is without question that there will be casualties. While we can do our best to mitigate loss of life and treat victims so they can return to their livelihoods, it is without question that some sort of pain management will be necessary for both the short and long term. Current practice relies heavily on prescription opioids to mitigate acute and chronic pain. These substances can be highly addictive, and if not used properly, carry potentially serious risks. By utilizing alternative pain management techniques such as ultrasound- guided nerve blocks, practitioners can effectively eliminate pain to targeted regions without any narcotic side effects, both increasing patient satisfaction and decreasing complication rates.
Background / Problems
In an effort to control pain, often-times opioid based medication is administered bedside and prescribed for continued use. This can easily be abused, become addictive, and carry the risks of many side effects including death. According to the US Dept of Health and Human Services 2017 survey, in 1 year alone, 42,249 people died from opioid overdose, with another 11.5 million people misusing their prescriptions (nearly 3x the amount of deaths compared to heroin). (“The U.S Opioid Epidemic”). According to the Center for Disease Control (CDC), from 2000-2015 over half a million people died from drug overdose. Due to the nature of military operations, studies have shown 60% of men and women returning from deployment suffer from some kind of chronic pain. The use of opioids as pain management coupled with the increased risk of depression/suicide/PTSD in veterans has led to US soldiers being 2x as likely to die from accidental opioid overdose (“Veterans Face Greater Risks Amid Opioid Crisis”). The effects of opioid dependency and abuse negatively impact both individuals from their day-to-day ability to function in society as well as a huge financial burden from supporting the pain management needs of our active duty and veteran warfighters.
According to the (“Report on Prescription Opioid Abuse and Effects on Readiness”), there is an active need for alternatives to opioid based pain treatments. “Initiatives include developing and implementing revised opioid prescribing guidelines and practices; mandating opioid prescriber safety training and educating providers to increase their use of non-pharmacological treatments for pain; and collaborating with other agencies on research into opioid addiction treatments, medication delivery systems that minimize diversion, and pain relievers with reduced misuse risk.” Combat medics’ current morphine sulfate auto-injector is the primary treatment option for pain management on the battlefield and other austere environments. Morphine cannot completely reduce pain, and it poses significant risks to wounded warfighters, including respiratory depression, hypotension, nausea, vomiting, and potential psychological and physical dependence.
Solution:
What if direct peripheral nerve blocks could be accomplished without any of the side effects seen in narcotic administration allowing a warfighter to maintain cognition and performance during triage/extraction? The recognition of the opioid epidemic became published in 2009. Since then, practitioners and researchers have been working to find ways to combat the issue including the use of epidurals to reduce the amount of needed morphine, mindfulness, acupuncture, and most recently used are ultrasound guided nerve blocks. The US Army has already seen the benefit of Ultrasound-Guided Nerve blocks in downrange applications adding in a course to the US Army Graduate Program in Anesthesia Nursing. With advancements in technology and ultrasound equipment becoming ultra-portable, we now have the ability to bring these techniques into combat and casualty care environments as well as all other echelon levels of care. (“New course teaches innovative techniques for pain management downrange”).
Ultrasound-guided nerve blocks can be used for immediate, direct pain relief, and they can also be used to place catheters for complete extremity blocks for multiple days at a time effectively treating those with less urgent triage categories or in austere prolonged field care environments.
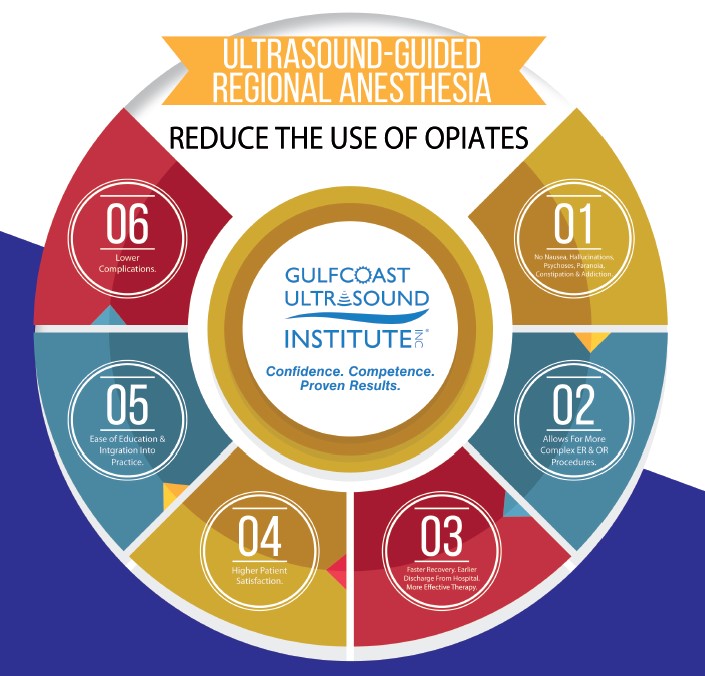
Along with reduction in side effects with reduced use of opioids, ultrasound guided nerve blocks are being shown to have significantly greater results in pain reduction / patient satisfaction (“Regional Anesthesia an Alternative to Opioids in the Emergency Department”).. While advanced ultrasound guided procedures like this can effectively treat and manage pain both in the battlefield and in prolonged care setting the skillset does take specialized training to master. Gulfcoast Ultrasound Institute (GSA Schedule contract holder GS-00F-103GA) offers live and online training programs specifically for Ultrasound Guided Regional Anesthesia (USGRA).
It is stated in (“Fundamentals of Combat Casualty Care, Ch3”). the uses of ultrasound in battlefield casualty environments such as FAST assessment, fractures, pneumothorax, vascular assessment, etc. When triaging and re-triaging casualty victims ultrasound can successfully be used for ultrasound guided nerve blocks allowing for non-urgent cases to be comfortable for longer periods.
Gulfcoast Ultrasound institute (GCUS) has been offering ultrasound specific training programs to military and civilian markets from around the United States for over 32 years utilizing expert faculty and live human patients. Select interventional courses also offer human cadaver workshops. GCUS offers courses live, online, or as custom on-site training programs for groups. Online courses provide users 12 months access to the lectures and activities from anywhere in the world on any device with an internet connection. An additional benefit for those in need is all programs offer AMA PRA Category 1 Credits.
Conclusion
Current pain mitigation protocol with casualty victims involves use of pre-metered morphine administration. Once issued, morphine will affect the patient's total mechanical and cognitive abilities, potentially causing more burden on the remainder of the team involved with the mission. If localized nerve blocks could be administered to casualty victims, not only would side effects with opioids be mitigated, the total efficiency of the team could be enhanced by having operators remain coherent and functional. While nerve block procedures can be done quickly and easily, adequate training is a necessity in being able to effectively integrate the ultrasound guidance into one's skillset. In addition to ultrasound guided nerve blocks, the same diagnostic equipment can be used for many other applications from combat and casualty care to prolonged care settings including: focused abdominal sonography in trauma, fracture assessment, ocular assessment, pneumothorax/hemothorax evaluation, and vascular assessment just to name a few. By arming operators with the tools and skills needed to implement ultrasound into practice, the quality, effectiveness, and speed of treatment can be greatly increased.
Works Cited
“The U.S. Opioid Epidemic.” HHS.gov, US Department of Health and Human Services, 21 Dec. 2017, www.hhs.gov/opioids/.
https://www.hhs.gov/opioids/about-the-epidemic/index.html
Childress, Sarah. “Veterans Face Greater Risks Amid Opioid Crisis.” PBS, Public Broadcasting Service, 28 Mar. 2016, www.pbs.org/wgbh/frontline/article/veterans-face-greater-risks-amid-opioid-crisis/.
Kurta, A. M. “Report on Prescription Opioid Abuse and Effects on Readiness.” Health.mil, Office of The Under Secretary of Defense, 29 Oct. 2017, health.mil.
https://www.gpo.gov/fdsys/pkg/CRPT-114hrpt537/pdf/CRPT-114hrpt537.pdf
Gerhardt, Robert T., et al. “Chapter 3.”Fundamentals of Combat Casualty Care, pp. 87–112.
http://www.cs.amedd.army.mil/borden/book/ccc/uclachp3.pdf
Sherner, John. “New course teaches innovative techniques for pain management downrange.” www.army.mil, US ARMY, 14 Oct. 2010, www.army.mil/article/46553.
https://www.army.mil/article/46553/new_course_teaches_innovative_techniques_for_pain_management_downrange
Ducharme, Jim. “Regional Anesthesia an Alternative to Opioids in the Emergency Department.” ACEP Now, American College of Emergency Physicians, 14 Apr. 2015, www.acepnow.com/article/regional-anesthesia-an-alternative-to-opioids-in-the-emergency-department.
US Army Institute of Surgical Research. “Battlefield Pain Management (BPM).” U.S. Institute of Surgical Research - Battlefield Pain Management, U.S. ARMY INSTITUTE OF SURGICAL RESEARCH, 30 Jan. 2015, www.usaisr.amedd.army.mil/05_bpm.html.
Gulfcoast Ultrasound Institute
www.gcus.com
111 2nd Ave. NE
Ste. 800
Saint Petersburg, FL 33701